New work in brain diseases like Alzheimer’s suggests that brain cells called neurons might be ‘catching’ the sickness from their neighbors. A recently published paper suggests that, in very specific lab conditions, this might also happen in Huntington’s disease. What does this mean for what we know about HD, and how to treat it?
Contagious brain diseases
In a family of brain illnesses we call neurodegenerative diseases, brain cells called neurons die, or ‘degenerate’. This family of diseases includes Huntington’s disease, but also other, more common, diseases like Alzheimer’s and Parkinson’s. In all these diseases, neurons die before they should, but each one blazes its own path of destruction – different parts of the brain are affected in each case.
This makes it interesting, but hard, to compare Huntington’s to these other diseases. Sometimes, things we learn in other condition apply to HD, but other features of each disease are unique. Every time someone discovers something unexpected in Alzheimer’s or Parkinson’s, you can bet that Huntington’s disease researchers scratch their heads and say “hmm, I wonder if that also happens in HD?”
Recently, scientists working in Alzheimer’s disease have been excited by a new set of observations centering on a tiny piece of the cell called the tau protein. The normal job of the tau protein is to help stabilize the skeleton of neurons – strengthening the long extensions that these cells reach out to one another.
After someone dies of Alzheimer’s disease, their brain shows different kinds of damage. One kind is made up mostly of a specific form of the tau protein. This fact, coupled with a lot of other information, has led scientists to believe that messed-up handling of tau protein is likely part of the process that leads to Alzheimer’s disease.
In a surprising set of experiments, scientists have recently shown that toxic tau proteins can be passed from one neuron to another, through their normal connections. This suggests an idea, not yet proven, that Alzheimer’s disease could start in one localized part of the brain and then spread to other, unaffected, regions.
It’s an attractive idea, because it could help explain the specific patterns of brain cell loss observed in Alzheimer’s disease.
Could HD be catching?
So, could this interesting thing observed in Alzheimer’s also occur in Huntington’s disease? In HD, the problem is not the tau protein, but rather the huntingtin protein – the product of the mutant huntingtin gene.
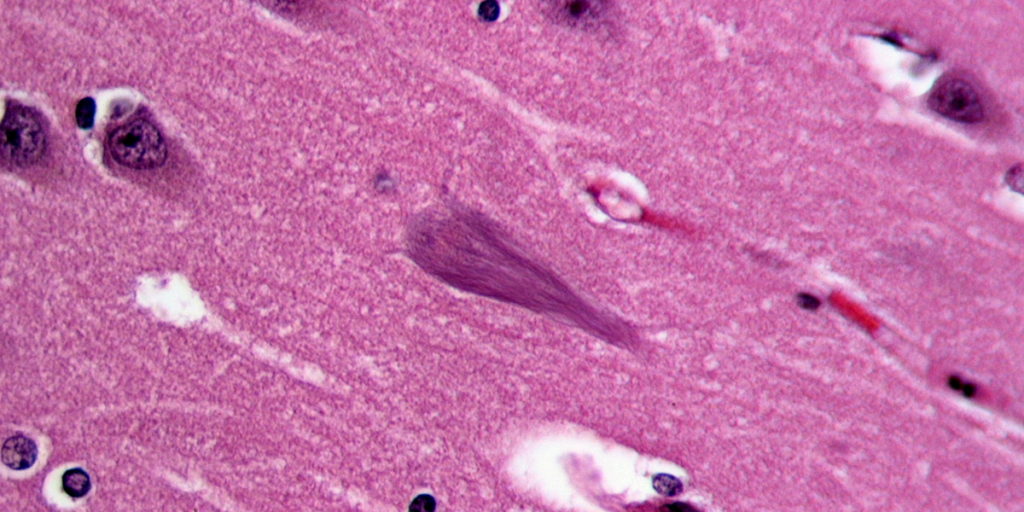
After death, the brains of Huntington’s disease sufferers are littered with clumps of stuff that shouldn’t be there, somewhat like in Alzheimer’s. In the case of HD though, those clumps are predominantly made up of the mutant huntingtin protein.
One question it’s useful to ask ourselves is: are there things about HD that we can’t explain without resorting to the idea that mutant huntingtin protein could be passed between cells? In Alzheimer’s, the specific pattern of cell loss observed was hard to understand, until this new contagious tau idea was hatched.
What mysteries in HD could this idea explain? Well, none that we know of, so far. Everything we know about HD fits into the pattern of cells in certain brain regions getting sick and dying. But that doesn’t mean it’s not worth checking to see if cells can, in fact, pass mutant huntingtin around.
New HD data
Scientists working at the Swiss drug company Novartis were interested in this question. They took advantage of some lab tricks, like growing normal human brain cells on top of slices of HD mouse brain. This is far from a normal situation for a neuron, but a very cool experimental setup to see whether stuff is getting passed from one cell to another.
In that particular experiment, the human neurons grown on top came from a person without an HD mutation, so they should never show these clumps of mutant huntingtin protein. But, after a few weeks of being attached to mouse cells with the mutant HD gene, the human cells seem to have ‘caught’ clumps of mutant huntingtin protein. The only possible source was the HD mouse cells below them.
Further work in whole mouse brains suggested that this curious result wasn’t merely a fluke caused by slicing the brain into sections.
What does it all mean?
This work clearly shows that, in specific lab conditions, mutant huntingtin protein can escape one cell and enter another one. What this work doesn’t tell us is whether this matters for real-life Huntington’s disease. Additional experiments are needed to prove whether this is just a funky lab phenomenon, or whether it’s a real part of the progression of a brain getting sick from HD.
If it is a real phenomenon that matters, this new finding could have big implications. Many of us are interested in the concept of replacing lost neurons with healthy new stem cells. But this new work suggests a major caution: it’s possible that healthy new cells we put in an HD patients brain could become ‘infected’ with mutant Huntingtin protein. Though it sounds a bit strange, something very similar has already been seen in the brains of Parkinson’s disease patients, whose healthy grafted stem cells became sick in a way that looks very much like their surrounding sick cells.
This is an important piece of work, that may help us understand the Huntington’s disease brain a bit better. It raises important cautions, which we can study in mice to help predict their significance in human HD patients! Look forward to more fascinating research in this area.