With gene silencing therapies heading towards the clinic, a new question has arisen – how will we know if they work? How can we tell if the amount of huntingtin protein is lowered in people? New work from London and Basel demonstrates that the huntingtin protein is detectable in blood samples, and that its levels change during the course of HD.
What’s so important about measurement?
One of the most fundamental ideas in science is that we have to be able to measure something before we can study it. How do we know if a drug works? We give it to a group of people, give another very similar group of people a sugar pill (“placebo”) and then measure some symptom in both groups of people. The drug is effective if people who got drug do better than those who got placebo.
Studies like PREDICT-HD, TRACK-HD and others have told us an enormous amount about what happens to people during the course of HD. We are ready, essentially, to pick sets of symptoms so that we can measure whether new drugs are effective or not.
But, on a deeper level-a scientist would say at the molecular level-how do we know that a drug is working in the way we think it should? In some cases, we can actually directly measure the actions of drugs.
For example, many millions of people take drugs called statins that prevent heart attacks by reducing the level of cholesterol in the blood. We can tell a statin is working, without waiting for heart attacks, by simply measuring cholesterol levels in the blood.
Every HD patient carries the same mutation in his or her DNA – a genetic stutter near one end of a gene we call the HD gene. Genes are used by cells as blueprints to create proteins – the machines that do most of the important work of our cells. The HD gene thus tells the body how to make a protein we somewhat confusingly call ‘huntingtin’.
One of the most exciting HD therapies on the horizon is gene silencing, which aims to lower the levels of the HD protein (huntingtin) in the brains of people carrying the HD mutation. Because we know that every single person who has HD has a mutation in the same gene, it’s easy to imagine this approach would be effective.
But how will we know whether the drugs we design to silence the HD gene actually work? In mice and other organisms we can just take brain samples from animals after they die and measure the levels of the huntingtin protein with standard lab techniques.
But there’s no way we can sample brain tissue from people participating in a gene silencing trial. It would be ideal if we could measure the levels of the huntingtin protein in samples that are easy to collect, like blood.
A group of scientists led by Prof Sarah Tabrizi at University College London and Dr Andreas Weiss at the pharmaceutical company Novartis set out to use a technique developed at Novartis to measure the HD protein in the blood of volunteers in the TRACK-HD study.
New technique enables novel questions
The team used a very sensitive technique called “Time Resolved Fluorescence Resonance Energy Transfer” or TR-FRET. The technique uses a pair of antibodies – which are proteins that stick to another specific protein – to label huntingtin.
The technical details are extremely complicated, but the basic idea is that when you zap one of the antibodies with a certain frequency of light, it causes the other antibody to emit light of a different frequency. The intensity of this different frequency of light tells us how much huntingtin protein is around. The benefit of this approach is that it’s very sensitive, which enables the team to measure the levels of huntingtin protein from very small volumes of biological samples, such as blood.
Tabrizi’s team has been interested for a long time in the activation of the immune system in HD. They’ve published work demonstrating that the immune system of HD patients seems to be hyperactive. This might sound like a good thing, but scientists know that too much activation of the immune system can be bad – and might even affect things happening in the brain.
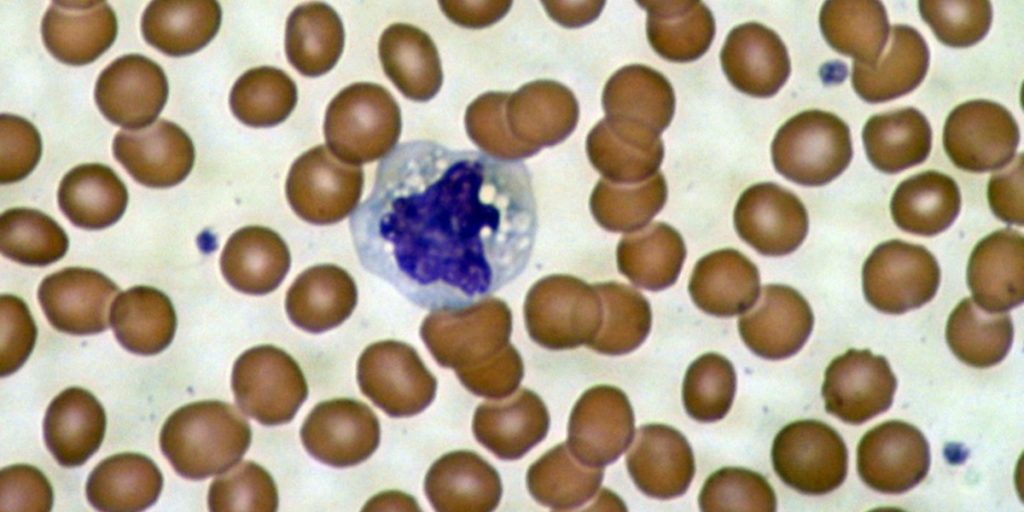
Given this interest and the ability to measure the huntingtin protein from small samples, the team set out to measure how much huntingtin protein there was in different types of cells in the blood of HD patients. Because the immune system is largely comprised of cells circulating in the blood, they reasoned that measuring huntingtin levels there might be useful.
What did they find?
What they found is interesting, and a bit perplexing. In different types of immune cells they found overall levels of the huntingtin protein were unchanged as HD progressed. This is a useful demonstration of their technique, and shows that they can accurately measure the levels of the huntingtin protein in cells from small blood samples.
The team then used different antibodies in their measurements, so that they only recognized the mutant form of the huntingtin protein. Remember, the vast majority of HD patients (and all the participants in this study) have two types of huntingtin protein – normal and mutant.
When they measured only the mutant form of the HD protein, the team observed increased signals in people who had shown HD symptoms longer. So it looks like people with more advanced HD have more mutant huntingtin in their immune cells in the blood. This finding is a bit surprising, but should we care about understanding what’s happening?
Brain/body connections
Here’s where the power of observational studies comes in. Because the team has been examining the volunteers who gave these blood samples, they were able to look for correlations between what was going on in their blood and how well the people were doing in terms of HD symptoms.
What they found is that higher levels of mutant huntingtin protein in the immune cells in the blood was clearly linked to having a higher burden of symptoms, and also associated with increasing brain atrophy. So, whatever is driving the increased levels of mutant huntingtin protein in blood cells, it’s likely worth understanding and could tell us something important.
Follow-up experiments suggest that what actually might be accumulating in the blood cells of HD patients are short fragments of the larger huntingtin protein. Previous work from a number of labs reveals that the huntingtin protein is cut up into small pieces, and that these small pieces might be especially toxic to the cell.
How is this useful?
This work is scientifically intriguing because it suggests that there could be accumulation and fragmentation of the huntingtin protein in the immune cells in the blood of HD patients. There are still some mysteries – what does the normal huntingtin protein do in these immune cells? Is the accumulation of mutant huntingtin protein related to the increased activation of the immune system in HD patients?
In terms of immediate benefit, this study demonstrates that it’s practical to measure the levels of normal and mutated huntingtin protein from very small samples, which is an important technical advance that will have many uses in HD research. Furthermore, this technique could be used to track levels of mutant huntingtin protein in the blood, which could provide a useful tool for scientists designing drug trials – particularly those focused on gene silencing.
A very exciting possibility that needs to be investigated further is whether the levels of mutant huntingtin protein in the blood reflect the levels of mutant huntingtin in the brain – essentially, does this offer a window into what is happening in the brain? If it does then this could be a very useful gauge of whether or not therapies that aim to lower levels of the mutant huntingtin protein in the brain are actually working.