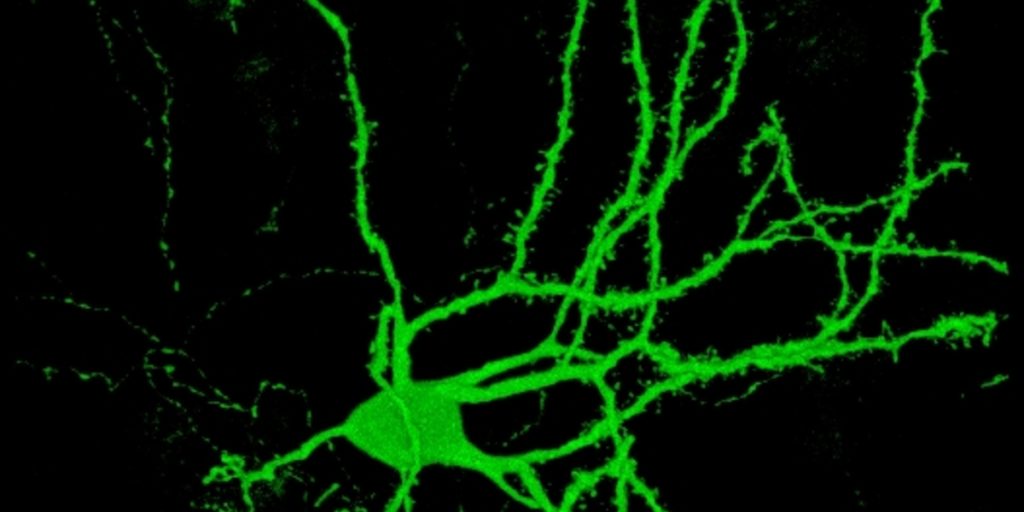
Scientists can now reprogram human skin cells to make working cells that resemble ‘medium spiny neurons’, the type of brain cell that is most affected early in Huntington’s disease. We’re still a long way off from being able to replace the brain cells that are being lost in HD, but this research is an important step down that path, and is a great tool to study HD.
Medium spiny what?
The medium spiny neuron is a type of brain cell that is affected early in Huntington’s disease. They make up about 96% of the striatum, a part of the brain that is important for the control of movement. This whole region is affected early on during the course of HD. Trying to replace the cells that are lost during HD is a goal for many researchers.
So, how do you make new neurons?
In 2006, Japanese researchers figured out a way to change the ‘instructions’ that a cell follows, so that it changes its cell type. Before this, it was thought that once a cell has committed to being a neuron, or a liver or skin cell, that decision can’t be changed. But in 2006 it became possible to turn adult skin cells into stem cells, which can then be coaxed into becoming any cell type.
Later, a group at Stanford University bypassed the stem cell step, and converted skin cells directly into neurons. That’s great but there are many different kinds of neuron, and Huntington’s disease researchers would love to be able to make medium spiny neurons.
Now, a team of scientists, led by Andrew Yoo at Washington University School of Medicine in St Louis, have done just that, by re-programming human skin cells. This work was recently published in the aptly named journal Neuron.
The usual approach to reprogramming of this kind is to baste the cells in a soup of chemicals called transcription factors. These tell cells which genes to switch on and off, eventually persuading them to change into a different cell type.
Yoo’s ‘secret ingredient’ was to add two micro molecules of RNA, a chemical cousin of DNA, along with the transcription factors.
It seems that the micro RNA was able to open up tightly-packaged bits of DNA, allowing the transcription factors to reach parts of the genetic code that a skin cell wouldn’t normally need to use. The micro RNA acted like a car jack, allowing access to the area that needs attention.
That was enough to make the cells start to look and behave like medium spiny neurons. They then transplanted them into mouse brains and, six months later, these reprogrammed neurons were behaving similarly to normal medium spiny neurons. They’d even started to reach out and grow into other areas in the movement control center of the brain.
Is this a treatment for HD?
Exciting though it sounds, so far this research hasn’t even started to look directly at the problem of Huntington’s disease directly. The mice that received the reprogrammed cells were just normal healthy mice, not HD model mice.
So, next the researchers have to check whether these reprogrammed neurons will perform just as well in HD mice, and whether they’ll have any effect on symptoms in those animals. Beyond that, it’ll require a further giant leap to apply these methods to human HD patients.
Transplanting new cells to replace those that are lost in a disease is known as cell replacement therapy. The cool thing about being able to use a patient’s own modified cells for therapy, is that the body’s immune system won’t reject the cells after the transplant, like it would for cells from another person.
However, since the mutation causing HD is found in every cell of our body, including our skin cells, any medium spiny neurons made from a patient’s skin will carry the mutation too. What we really want is a source of healthy cells that aren’t vulnerable to the harmful effects of the HD mutation.
So, before these techniques could lead to a cell replacement therapy, we will first need to figure out how to remove the HD mutation from them. New technologies with names like ‘genome editing’, ‘zinc fingers’ and ‘Crispr’ may be able to do this in future, but they are still being fine-tuned for this use. It’ll take years of careful research before these methods are ready to test in humans.
Finally, important though medium spiny neurons are, they are not the only brain cell involved in Huntington’s disease. Ideally, we’d like to replace all the lost or malfunctioning cell types – each one needing its own recipe and detailed study, followed by even more research to get the different cells working together.
What about now?
The road to treatments here is long, but research is already underway with multiple teams working on these important areas.
More good news is that this work done by Andrew Yoo’s team will have immediate use to Huntington’s disease researchers. This new way of growing medium spiny neurons from HD patients will help us understand why these neurons are so vulnerable in HD. They can also be used to test new drugs for HD right away, to help us develop the best drugs to test in people.